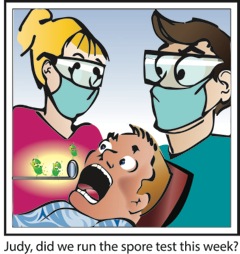
Sterilization monitoring is a critical component of infection control in dental practices. One of the…
CDC Guidelines: Sterilizing Heat-Sensitive Dental Instruments – Dental Infection Control
The Centers for Disease Control and Prevention (CDC) categorizes patient-care dental items (instruments, devices, equipment) into three categories:
- Critical items cut bone and/or penetrate soft tissue and carry the highest risk of disease transmission.
- Semi-critical items touch mucous membranes or nonintact skin. They have a lower risk of disease transmission.
- Non-critical items contact intact skin, and have the lowest risk of disease transmission.
According to the CDC, all patient-care items must be cleaned prior to sterilization. Following cleaning, heat-stable critical and semi-critical dental instruments must be heat sterilized before each use.
But what if the dental instrument is not compatible with heat, which is considered the gold standard method of sterilization in a dental office?
Heat-sensitive critical items must undergo cold sterilization while semi-critical items must at least undergo high-level disinfection. Heat-sensitive critical and semi-critical items can be processed by immersing them in liquid chemical germicides approved by the Food and Drug Administration (FDA) as sterilants or high-level disininfection. FDA-cleared chemical sterilants include glutaraldehyde, hydrogen peroxide, peracetic actid, and ortho-phthaldehyde (high level disinfection only).
Shorter immersion times of the FDA-cleared chemicals can be used to achieve high-level disinfection of semi-critical instruments only. Note that chemical contact time is the single critical variable distinguishing the sterilization process from high-level disinfection.
CDC strongly recommends that whenever possible, heat-stable items be used instead of those that are heat-sensitive because limitations exist with using chemical sterilization because:
- Post-sterilization of heat-sensitive items, the items need to be 1) rinsed with sterile water to remove chemical residues, 2) dried with sterile towels, 3) packaged or wrapped, 4) and handled using sterile gloves.
- If stored before use, the items must be sterilized again just before use.
- The sterilization process with cold sterile solutions cannot be verified with biological indicators.
- Sterilization of heat-sensitive items requires up to 12 hours of complete immersion, and therefore are usually only used for high level disinfection of semi-critical items.
- Manufacturer label instructions and safety precautions must be followed carefully. Misapplications include use as an environmental surface disinfectant or instrument holding solution.
- Chemical sterilants are highly toxic, and require appropriate precautions – closed containers, proper PPE – chemical-resistant gloves and aprons, safety eyewear, face shields, safe chemical handling.
Using heat-sensitive items that must be processed with liquid chemical germicides is discouraged; heat-tolerant or disposable alternatives are available for the majority of such items. Contact the manufacturer to make sure your “heat-sensitive item” is, in fact, heat-sensitive.
Since 1992, OSHA Review, Inc. has provided dental professionals with comprehensive programs to support regulatory compliance and infection control. We are a registered continuing education provider in the state of California, specializing in Dental Practice Act, infection control, and OSHA training.